
What is varicose veins and how does it manifest? What happens if you don't treat varicose veins and how can you prevent them? We talk about complications of varicose veins, explain in detail why trophic ulcers occur and why compression stockings are needed.
What is varicose veins and how does it manifest?
Veins have special valves that prevent blood from flowing down the vessel. But with varicose veins, these valves don't close completely -- blood builds up in the vein and stretches it.
Symptoms of early varicose veins:
- The veins in the legs become brighter and more visible;
- On the inner surfaces of the legs and thighs, varicose veins begin to appear;
- Legs feel heavy and full if you stand, sit, or walk for long periods of time (most often at night, calves);
- Pain or severe pain in the evening and at night where the veins are dilated - muscle spasms in the calf;
- By the end of the day, the leg will be very swollen, but by the morning the swelling will go away.
important!
Already at this stage, it is necessary to consult a doctor.
As it progresses, varicose veins become chronic (chronic venous insufficiency). symptom:
- Intensely tortuous dark blue intradermal veins: they protrude above the surface of the legs and feet and look like a bunch of ripe red grapes;
- Bow pain in the legs and calves, heat in the legs, cramps in the calf muscles at night, and severe swelling;
- The skin becomes dry, hyperpigmented, darkened, and brown spots appear.
important!
Do not cause disease! Varicose veins disrupt tissue nutrition. Blood vessels and skin are not getting enough nutrition - wounds, eczema or even ulcers appear and heal poorly.
Treat varicose veins
There are two ways to treat varicose veins: conservative treatment and surgery.
- Conservative: compression therapy. Compression underwear squeezes the affected leg - the diameter of the superficial veins decreases, restoring the correct pressure in the veins. Blood backflow is reduced, vessel walls remain in good condition, valves close, blood is not stagnant and circulates well, and the velocity of blood through deep veins increases. The amount of stagnant blood is reduced and the lymphatic outflow is improved.
- In advanced cases, when conservative treatment doesn't help, doctors recommend a surgical route: excision of the varicose veins, removal of the affected veins. To restore function, place a shunt or restore the valve's mobility so that its leaflets close.
Compression knitwear for varicose veins and ulcers
Compression stockings are special stockings that fit snugly against the calves and become looser as they rise to the thighs. This improves circulation and stimulates blood flow from the lower extremities to the heart.
Compression stockings are individually selected, so check with your phlebologist first: you cannot choose compression stockings on your own.
The phlebologist will look at the tone of the veins where a particular valve has a problem with the valve not closing. For example, the problem may be in the thighs: then you need to wear compression stockings. If closing the valve below the knee is a problem, opt for socks or stockings.
important!
For maximum effect, wear compression stockings at all times - take them off only before bed.
How to put on compression stockings?
- When you wake up, put your legs on the wall and lie like this for a while - to get the blood flowing to your buttocks as much as possible;
- Don't get up, put on compression stockings.
In this position (lying down, legs raised), the blood flows evenly and the blood does not stagnate. When compression stockings are worn on the legs, the veins are in good shape and the valves close well, pushing blood further through the vessels.
What happens if varicose veins are not treated?
If treatment for varicose veins is not started promptly, life-threatening complications can occur:
thrombophlebitis- Inflammation of the veins due to the formation of blood clots in them. symptom:
- redness;
- the place where the blood clot is located becomes warm;
- Inflamed veins are painful.
If treatment is started in time, the thrombus will stop growing. Residual blood clots can go away for a long time—sometimes months. Clots can grow if left untreated or handled improperly.
Pulmonary embolism.The blood clot that occurs with thrombophlebitis breaks off the walls of blood vessels in the legs and leaves with the bloodstream. It blocks the pulmonary artery or its branches - which is fatal. Unfortunately, even if this complication is suspected in time, there is little doctors can do.
symptom:
- chest pain;
- Heartbeat;
- Difficulty breathing;
- Unreasonable anxiety and unreasonable fear.
Deep vein thrombosis of lower extremity. This is a serious and dangerous complication of varicose veins. The internal veins are blocked, therefore, the outflow of blood is almost completely stopped - all the tissues of the leg are not nourished, it turns blue.
Venous gangrene of the extremities- Severe deep vein thrombosis in which the limb is not nourished and arterial blood flow is disturbed. As the blood does not flow, gangrene develops: in fact, the leg is dead - starting with the fingers.
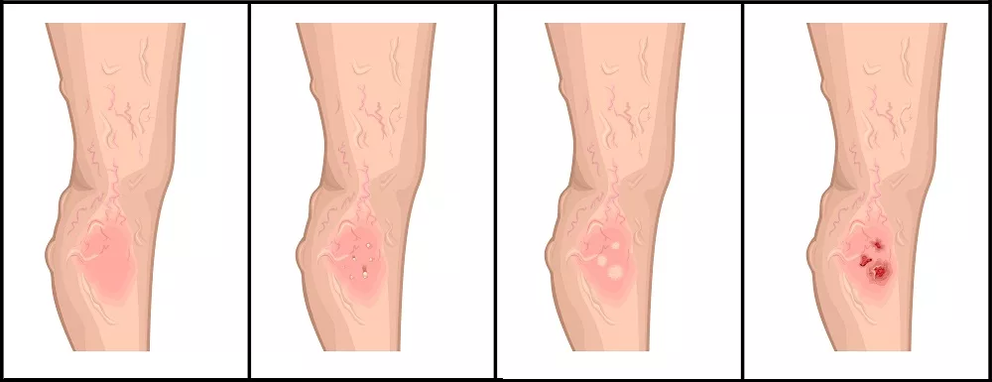
trophic ulcer- Prolonged non-healing ulcers due to tissue malnutrition. Lymph is trapped in the lymphatic vessels and they are under a huge load and cannot cope with the amount of lymph. As a result, the lymphatic droplets begin to protrude through the skin. Because of this, the epidermis begins to peel - forming ulcers with jagged edges. Any touch it causes severe pain.
Bacteria develop rapidly in the ulcer: the infection joins, and the bleeding ulcer begins to fester. This can lead to very serious complications, including blood poisoning.
There are two types of trophic ulcers:
- veins, when the subcutaneous and deep veins of the limb are affected;
- Arteries, when the arteries in the legs are affected and the natural nutrition of the extremities is disturbed.
Treatment of nutritional ulcers
Nutritional ulcers are treated with elastic compression, drugs, physical therapy, and surgery.
Nutrient ulcer care consists of four stages.
Stage 1 - Preservatives
- Antiseptic solution for wound treatment. It is applied to the surface of trophic ulcers, and if cavities have formed under the skin, they are also filled with gel.
- The gel is antibacterial and anti-inflammatory, improves microcirculation, reduces skin redness and swelling, relieves pain, relieves itching and flaking, stops infection from spreading and prevents scarring.
- Aqueous solution of halogen or benzyldimethyl-myristoylamino-propylammonium preservative.
Stage 2 - Gel to soften dead tissue
Dead tissue is necrosis: black hardened tissue on the surface of the ulcer. The ulcer will not heal if it is not removed. To do this, first soften the necrosis. This is done using a special gel.
The third stage is the formation of the optimal environment for wound healing
Promotes healing by creating a moist environment in the wound. If there is no necrosis, use a bandage to heal quickly. Here are some suitable bandages:
Alginate Dressing:
- An alginate dressing that turns into a soft gel upon contact with wound secretions, providing optimal conditions for wound moist healing;
- A dressing that fills the wound cavity and creates a microenvironment that promotes rapid healing;
- Sponge bandage with hydrogel layer. Its structure absorbs secretions and maintains a moist environment in the wound;
- Alginate sponge dressing composed of calcium alginate and hydrocolloids;
- Self-absorbing sterile coating based on sodium alginate, ideal for wounds and burns, accelerating healing;
- Hydroactive dressing for deep wounds. Cleans wounds, accelerates their healing, and maintains optimal wound conditions for up to three days without changing dressings.
Sponge Bandage:
- Double-sided foam bandage. It protects the wound, absorbs wound secretions and creates an optimal water balance in the wound;
- Hydrophilic polyurethane sponge dressing;
- A dressing containing a complex of enzymes and chitosan is suitable for infected wounds (if the wound has pus);
- An antibacterial sponge breathable dressing is composed of a sponge polyurethane layer and a silver alginate matrix.
Stage 4 - Wound Healing
When a wound is cleaned and an optimal environment is created in it, it begins to heal and the wound edges shrink. For safe and fast healing, use special dressings.
Mesh Ointment Bandage:
- Apply a Peru Balsam ointment dressing when fresh skin appears on the wound;
- Ointment dressings based on triglycerides to promote healing and care for wound edges;
- The bandage looks like a wax cube and is soft and very dense. Can be on the wound for up to 7 days;
Film dressings that can be used to secure wound dressings:
- Membrane (but breathable) waterproof bandage that protects the wound from microbes. It can be used to hold previous bandages in place, or it can be used as a standalone bandage.
- Transparent film polyurethane bandage, the skin under it does not sweat and breathes.
important!
These dressings are suitable not only for the treatment of trophic ulcers, but also for any long-term healing wound.
prevent varicose veins
- Move as much as possible: the more you move, the better the circulation of blood in the veins;
- Get rid of bad habits;
- Contact a phlebologist promptly at the first symptoms of the disease;
- Regular ultrasounds of blood vessels - doctors will notice initial changes;
- After a long day at work, come home and put your feet on the wall for about 15 minutes.
Prevention of nutritional ulcers
- Watch your weight: it puts pressure on your legs and increases the load on your blood vessels and lymphatic system. follow a diet if necessary;
- walk as much as possible;
- If possible, lift your legs and keep them as elevated as possible. At night, you can lie on the sofa with your legs raised and put it on the wall: you need to lie there for at least 15 minutes;
- Prompt treatment of lower extremity veins;
- quit smoking - it greatly reduces the blood supply to the tissues and leads to the development of trophic ulcers;
- Take care of your feet: wear suitable shoes so they don't sting or rub;
- Check your feet regularly: Check the color of the skin on your feet. If your legs turn blue at night and veins are visible in your legs, contact your phlebologist;
- Moisturize your skin with a soft, moisturizing, nourishing cream;
- keep your feet warm and dress for the weather;
- Try not to damage the skin.


















